Even before we had discovered vitamin C, we knew that there was something in fresh fruit and vegetables that kept us healthy. Medical textbooks dating as far back as ancient Egypt describe a treatment of fresh vegetables to cure symptoms of the vitamin C deficiency disease, scurvy [1]. Scurvy was a scourge throughout history. For thousands of years, scurvy was endemic in Northern Europe in the winter and early spring, and in populations that had to consume a diet lacking in fruits and vegetables, such as soldiers and sailors, prisoners, and in besieged towns [2]. Symptoms have been described in medical textbooks dating back thousands of years. Deficiency signs appear after a few weeks of a lacking diet, and include malaise, bone and muscle pain, changes in the appearance of the skin, easy bruising, poor wound healing, and gum disease [3]. Eventually, scurvy is fatal. The disease changed history, halting naval and military expeditions, and was the cause of the failure of some attempts to colonize the New World [1, 4].
Nowadays, we know what causes scurvy and how to prevent and treat it. Sufficient intakes of vitamin C prevent deficiency. Treatment of scurvy involves dosing large amounts orally for a few weeks until symptoms resolve [5], then addressing the cause of low vitamin C intakes. Even so, scurvy still appears regularly in case reports in the medical literature, usually caused by problems with chewing food, food fads that lead to vitamin C-poor diets, various gastrointestinal diseases that reduce vitamin C absorption, and alcohol abuse [6]. Most surprising have been reports that a biochemical vitamin C status indicative of deficiency is fairly widespread. The overall prevalence of vitamin C deficiency in the US is 7%, with higher rates seen in adult men, smokers, and people of lower socioeconomic status [7]. For example, nearly one in five male smokers are likely to be vitamin C deficient [7]. A similar pattern is found in the UK, where approximately 25% men and 16% of women in materially deprived social strata are vitamin C deficient [8].
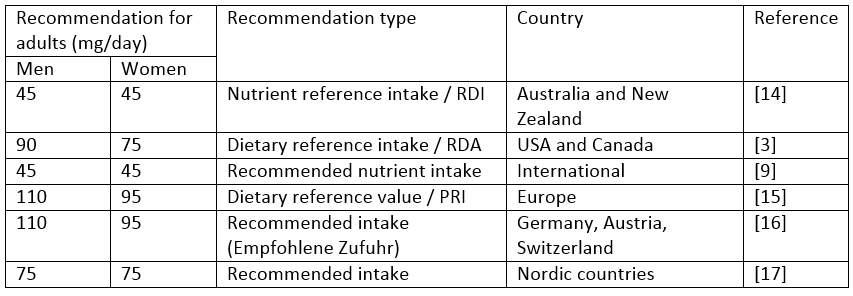
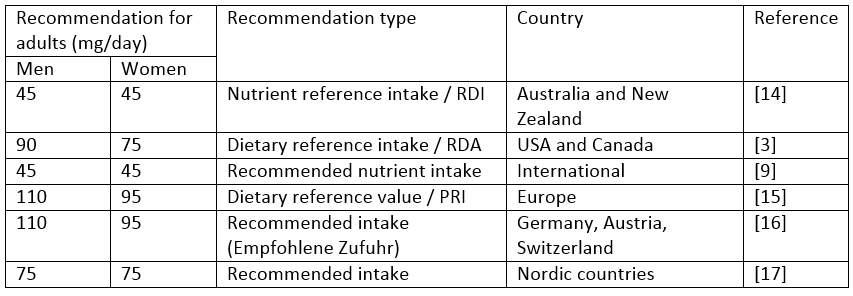
Despite the widespread knowledge of vitamin C deficiency, there is considerable variation in recommendations that differ more than two-fold depending on the country issuing the nutrition advice (see table). The European Food Safety Authority (EFSA) recommends that adult men consume 110 mg vitamin C per day, and the recommendation for women is a little lower due to their smaller body size. When recommendations from the World Health Organization (WHO) are consulted, however, recommendations are less than half this at 45 mg for an adult per day, regardless of gender. The differences arise from the way that the recommendations were calculated. The approach used by the WHO is based on the amount needed to reach total body stores halfway between deficiency and saturation (900 mg), assuming that the body uses 26 mg per day, and that absorption is 85% of intake [9]. EFSA on the other hand assumes that the body uses 50 mg per day, only 80% is absorbed, and that urinary excretion is around 25% of intake. Added to this is a certain margin to ensure that most people will consume enough, and the higher recommendation of 110 mg per day is reached.
The WHO and the Institute of Medicine (IOM) provide information on intakes that cause undesirable effects. The WHO found that intakes of greater than 1,000 mg per day may cause some gastrointestinal distress as unabsorbed vitamin C can irritate the lining of the intestine. Kidney stone formation may also increase at intakes over 1,000 mg per day over an extended period of time [9]. The IOM set a Tolerable Upper Limit of 2,000 mg per day due to gastrointestinal complaints [3].
The reports from both these organizations cite the intake at which tissue saturation is reached: 200 mg per day. This is based on a vitamin C depletion and repletion study performed to aid the establishment of an RDA [10]. The researchers found that the relationship between vitamin C levels in the body and intakes are an S-shaped curve. At low intakes, the body attempts to maintain a minimum level of vitamin C in the body. There is a large response in tissue levels when intakes increase. At intakes of around 60 mg per day, the curve starts to flatten out, which means that there are only small increases in plasma concentrations as intakes increase above this amount. The authors recommend an intake of 200 mg as it corresponds to the lowest intake associated with adequacy. Intakes above 400 mg do not result in any increase in tissue levels. The authors of the article state clearly that they recommend an intake of 200 mg per day for healthy young men. Another vitamin C depletion study was performed in healthy young women – a similar pattern was found although intakes of 90 mg were considered sufficient for women [11].
Two similar studies were repeated in larger and more diverse groups of older men. One study was a repeated depletion-repletion study that showed considerable variation in response to a vitamin C dose of 120 mg per day [12]. Around half the subjects did not achieve plasma vitamin C concentrations that correspond with adequacy (> 50 µmol/L) after one month of 120 mg per day vitamin C. Body weight differences were identified as a key cause of differences in how well plasma vitamin C increased after supplementation, namely that subjects with a greater body weight did not have as strong an increase in vitamin C concentrations. The second study, a retrospective analysis of studies conducted by one research group, found that consumption of 50 mg daily on top of an average intake of 25 mg per day did not normalize vitamin C levels in 15% of subjects that entered the study with marginal deficiency, although 200 mg per day (provided either by a supplement or two kiwi fruits) did [13].
The results from these carefully controlled depletion studies indicate that intakes within the current range of recommendations (45 to 110 mg per day) will not result in saturation of plasma vitamin C concentrations for most people. The lower intake recommendations in Australia/New Zealand, and from the WHO, place a considerable proportion of the population at risk of deficiency. Even if this does not result in overt scurvy, non-specific symptoms of marginal deficiency such as fatigue and depressed mood affect quality of life [13]. The mismatch between intakes and plasma levels arises from the calculations used to estimate vitamin C balance: they are probably not sufficient to capture the full range of responses to vitamin C intakes seen in the free-living population. Various factors including genetics, gastrointestinal integrity, body weight, and oxidative stress (such as has already been confirmed for cigarette smoking) affect the need for vitamin C [13]. The aging population and issues with dentition, plus the obesity epidemic, further increase the need for vitamin C in general. Consuming five servings of fruit and vegetables per day is adequate to meet intake recommendations up to 200 mg per day, and vitamin C supplements are widely available at a low cost for people unable or unwilling to meet recommendations with food.
Nutrient intake recommendations are a guide for public health professionals, dietitians, and food producers. They affect individuals’ behaviors. Current recommendations should be reassessed to ensure that they are adequate to reduce the prevalence of frank and marginal vitamin C deficiency.
Table: Dietary intake recommendations for vitamin C