News
Fish-rich diet may decrease risk of heart disease in women
27 December 2011
According to a new Danish study, increased intakes of fish rich in omega-3 fatty acids may help protect young women from heart disease.
01 March 2011
Cardiovascular health relates to the health of the heart, the blood vessels and the organs that are critically dependent on a strong blood supply. A smoothly functioning cardiovascular system is crucial to good overall health as every cell of the body depends on its function for survival. Accordingly, disorders of the cardiovascular system can have far-reaching effects.
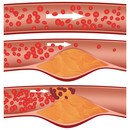
 The main underlying causal mechanism of cardiovascular disease is atherosclerosis, a condition which is typically asymptomatic for decades, in which artery walls thicken as the result of a build-up of fatty materials. Over time, arteries harden and become narrowed, limiting the flow of oxygen-rich blood to the organs and other parts of the body. This can lead to serious health problems such as heart attack, stroke, or even death. Much of the health and economic burden of cardiovascular disease can be prevented and controlled through increased physical activity, maintaining a healthy body weight and eating a balanced, micronutrient-rich diet.
The main underlying causal mechanism of cardiovascular disease is atherosclerosis, a condition which is typically asymptomatic for decades, in which artery walls thicken as the result of a build-up of fatty materials. Over time, arteries harden and become narrowed, limiting the flow of oxygen-rich blood to the organs and other parts of the body. This can lead to serious health problems such as heart attack, stroke, or even death. Much of the health and economic burden of cardiovascular disease can be prevented and controlled through increased physical activity, maintaining a healthy body weight and eating a balanced, micronutrient-rich diet.
 The cardiovascular system transports food, hormones, metabolic wastes, and gases (oxygen, carbon dioxide) to and from cells. Components of the system include blood (consisting of liquid plasma and cells), heart (a muscular pump to move the blood) and blood vessels (the "channels" which carry blood to/from all tissues). The arteries are strong, elastic vessels adapted for carrying oxygen-rich blood away from the heart at relatively high pumping pressure. They use vessel size (dilation and constriction), controlled by the nervous system, to move blood by pressure. Veins return deoxygenated blood to the heart and carry it to the lungs where blood is oxygenated before it returns to the heart. Arteries and veins run parallel throughout the body with a web-like network of capillaries connecting them. Capillaries are thin-walled blood vessels in which the exchange of gases, nutrients, and wastes between the blood and surrounding tissues occurs.
The cardiovascular system transports food, hormones, metabolic wastes, and gases (oxygen, carbon dioxide) to and from cells. Components of the system include blood (consisting of liquid plasma and cells), heart (a muscular pump to move the blood) and blood vessels (the "channels" which carry blood to/from all tissues). The arteries are strong, elastic vessels adapted for carrying oxygen-rich blood away from the heart at relatively high pumping pressure. They use vessel size (dilation and constriction), controlled by the nervous system, to move blood by pressure. Veins return deoxygenated blood to the heart and carry it to the lungs where blood is oxygenated before it returns to the heart. Arteries and veins run parallel throughout the body with a web-like network of capillaries connecting them. Capillaries are thin-walled blood vessels in which the exchange of gases, nutrients, and wastes between the blood and surrounding tissues occurs.
A strong, healthy heart is vital for longevity. The heart beats around 70 times per minute and undergoes over 3 billion contractions during a normal lifetime. The hard-working muscle needs a consistently sufficient blood and oxygen supply. Healthy blood vessels are elastic and flexible, accommodating blood flow changes due to physical activity and stress levels. The better the tone of the blood vessels the less the heart has to work to pump blood. Since an efficient working heart and vascular system are essential for all body functions, cardiovascular diseases can impact overall health. The term "cardiovascular disease” generally refers to conditions that involve narrowed or blocked blood vessels that can lead to a heart attack (blood supply is cut off from a part of the heart), angina pectoris (chest pain caused by too little blood and oxygen supply of the heart) or stroke (disturbance in the blood supply to the brain).
Cardiovascular disease is the No. 1 worldwide killer of men and women (1) with global healthcare costs of over USD 500 billion (2). The main underlying mechanism is atherosclerosis, a condition in which an artery wall thickens as the result of abnormal build-ups of fatty materials such as cholesterol and a chronic inflammatory process in the inner lining of the arteries (3). As a consequence, multiple plaques are formed within the arteries causing a loss of their elasticity (hardening) and reducing their interior (narrowing). This can lead to a restricted or even blocked blood flow to organs and tissues.
By the time cardiovascular problems are detected, atherosclerosis is usually quite advanced, having progressed asymptomatically for decades. Thus, there is increased emphasis on preventing atherosclerosis by modifying the major risk factors: unhealthy diet, insufficient physical activity and tobacco smoking (4). A nutritious, balanced diet can significantly lower the chances of developing cardiovascular diseases, as well as help to manage existing heart disease. By incorporating certain micronutrients into the diet, cardiovascular health can be improved and maintained.
 Promoting heart function
Promoting heart function
The most obvious signs of heart malfunctioning are intense chest pain (angina pectoris) or an unstable heart rhythm. A high heart rate (heartbeats per minute) and heart rate variability are independent risk factors for cardiovascular death, particularly sudden death. Micronutrients can help maintain heart function and reduce the risk of heart disease.
Large observational studies and clinical intervention studies showed that omega-3 long chain polyunsaturated fatty acids can reduce the risk of coronary heart disease. A meta-analysis recently showed that omega-3 fatty acids can reduce heart rate (5). Omega-3 fatty acids also lowered heart rate variability in several clinical studies. This effect is most likely due to the PUFA (Poly Unsaturated Fatty Acids) being incorporated into cell membranes, improving cell-to-cell communication (6).
Another direct cause of heart failure is the inability of cells in the wall of the heart to provide the heart muscle with enough energy for it to function effectively. Coenzyme Q10 may increase the efficiency of energy production in these vital heart cells. Clinical studies have shown CoQ10 to consistently improve cardiac parameters, such as the amount of blood the heart can pump, in chronic heart failure (7).
 Improving blood lipids
Improving blood lipids
Cholesterol, a fat-like substance consisting of fatty acids, long chain alcohols and different sugar residues, is essential for the formation of sex hormones, bile salts and vitamin D, and is a building material for cell membranes. Since cholesterol and other fats cannot dissolve in the blood, they have to be transported to and from the cells by special carriers called lipoproteins. Low-density lipoprotein (LDL) is the major cholesterol carrier in the blood. If too much LDL and very low-density lipoprotein (VLDL) cholesterol circulate in the blood, they can slowly build up in the artery walls (plaque formation) leading to atherosclerosis and increasing the risk of heart disease. About one-third to one-fourth of blood cholesterol is carried by high-density lipoprotein (HDL). HDL is thought to carry cholesterol away from the arteries and back to the liver, where it's passed from the body. In addition, HDL seems to remove excess cholesterol from plaques, protecting against heart disease. Triglycerides are the most common type of fat in the body. There is strong evidence that they are also an independent risk factor for heart disease. Elevated blood triglyceride levels appear to interfere with the normal widening of the arteries that occurs during physical exertion. Getting the balance right between HDL and LDL cholesterol, and reducing triglycerides and VLDL, are important ways to lower the risk of cardiovascular disease.
Numerous clinical studies show that omega-3 long chain polyunsaturated fatty acids dose-dependently lower plasma triglyceride levels (8). They are thought to work by reducing production of triglycerides and VLDL in the liver (9). They can also increase HDL- cholesterol concentrations and improve the LDL/HDL ratio (10).
High blood homocysteine levels have been linked to an increased chance of developing heart disease. The vitamins B2, B6 and B12, and particularly vitamin B9 (folate), have been shown to lower homocysteine levels. Thus, people with sub-optimal B vitamin intake may be able to reduce their risk of cardiovascular disease, in particular stroke, by increasing their consumption of B vitamins (11).
 Preventing LDL cholesterol oxidation
Preventing LDL cholesterol oxidation
LDL cholesterol is the main carrier of fats and oils in the blood. When LDL becomes oxidized, it sets off a chain reaction that produces compounds in the blood that damage the artery wall and begin the process of atherosclerosis (12). Studies show that people who eat a diet rich in antioxidant micronutrients have a lower incidence of heart disease (13). These high circulating levels of antioxidants may reduce the effects of oxidation and prevent the damage caused by oxidized LDL cholesterol (14).
As an important fat-soluble antioxidant vitamin E has been shown to reduce the oxidation of LDL cholesterol, involved in the build-up of plaque in the arteries (15). Population studies have shown that vitamin E could be protective against coronary heart disease (16, 17). In addition, vitamin E may contribute to reducing cardiovascular mortality in specific high-risk groups of the population (18, 19).Vitamin C helps regenerate vitamin E to keep it performing as an antioxidant.
Lycopene, a nutrient naturally occurring in tomatoes, is a potent antioxidant. Population studies have shown that people who consume a large amount of tomatoes and tomato products, rich sources of lycopene, have a lower incidence of cardiovascular disease. Lycopene reduces LDL-cholesterol oxidation, and preliminary evidence suggests that it may prevent cardiovascular disease (20).
 Promoting healthy blood pressure
Promoting healthy blood pressure
High blood pressure (hypertension) makes the heart work harder than normal, causing it to enlarge and weaken over time. It places stress on blood vessels and can damage them. Preventing high blood pressure can help to avoid detrimental damage to the arteries and heart, as well as to other organs like the brain.
Clinical and observational studies suggest that vitamin C plays an important role in blood pressure regulation. A high intake of vitamin C from food may protect against raised blood pressure and strokes (21). Vitamin C supplementation has been shown to lower blood pressure, and to reduce the stiffness of the artery walls (22-24).
Population studies link low concentrations of vitamin D with an increased risk of cardiovascular disease, particularly heart attack (25, 26) and hypertension (27-29). Increasing evidence indicates that enhancing the circulating levels of vitamin D can reduce hypertension incidence, helping to maintain a healthy blood pressure (30). Lower levels of vitamin D and higher levels of calcium appear to be associated with different cardiovascular risk factors and may therefore affect cardiovascular disease risk through different mechanisms.
Coenzyme Q10 is involved with energy generation in cells, and is found particularly in metabolically active organs like the heart. It is produced by the human body, but levels decline with age and with some medications. CoQ10 is thought to preserve the availability of nitric oxide, a signaling molecule that helps blood vessels to dilate. CoQ10 consistently reduced blood pressure in a number of long-term studies (31).
High doses of omega-3 fatty acids have been shown to lower systolic and diastolic blood pressure in hypertensive subjects. The effect was dependent on the degree of hypertension. A meta-analysis found a significant reduction in blood pressure in hypertensive subjects who consumed a high level of omega-3 fatty acids (32).
The minerals potassium and magnesium can also help to maintain healthy blood pressure (33, 34).
 Promoting healthy blood vessels and circulation
Promoting healthy blood vessels and circulation
For the blood circulation to function properly, blood needs to flow freely without obstruction through the blood vessels. The system malfunctions when the blood vessel tone is not adequate or blood cells stick together (platelet aggregation), causing blood clots that can lodge in the veins and arteries (35). The concept of improving blood vessel tone centers on the endothelium, a thin layer of cells that line the inside of the blood vessels. Endothelial cells are major players in regulating blood flow, blood pressure and clotting. The cells secrete a variety of chemicals that signal blood vessels to dilate and constrict, which helps regulate blood flow, as well as to activate cells involved in blood coagulation. Endothelial dysfunction has been identified as a major risk factor for coronary heart disease (36). Elevated blood levels of oxidized-LDL cholesterol, triglyceride and homocysteine have been suggested to increase the chances of having endothelial dysfunction.
Some studies have suggested benefits of the antioxidant vitamins C and E in improving endothelial function in healthy subjects (37), high risk groups (38, 39) and cardiovascular patients (40). In addition, trials indicated that the vitamins could prevent an impaired function caused by elevated blood levels of homocysteine (41). This ability to maintain normal blood vessel tone by reducing vascular oxidant stress may partly account for the vitamins’ benefits in preventing cardiovascular diseases.
A growing body of evidence indicates that increased intakes of vitamin K may reduce the build up of calcium in arteries that leads to hardening of the blood vessels. A study found that supplements of vitamin K1 may slow hardening of the arteries in people already suffering from the condition (42).
A recent study showed that vascular endothelial function seems to be related to the vitamin D status: lower blood vitamin D levels were associated with vascular endothelial inflammation (43). In addition, vitamin D supplementation has shown to be effective in improving vascular endothelial function (44).
Dietary omega-3 fatty acids are incorporated into the cell membrane, putting them in the right spot to reduce platelet aggregation (45). From here they shift the production of thromboxane, a lipid responsible for blood clotting, to a less potent form (9).
27 December 2011
According to a new Danish study, increased intakes of fish rich in omega-3 fatty acids may help protect young women from heart disease.
30 January 2013
According to a new study from Canada, the two factors most strongly associated with higher vitamin D levels in young children are taking a daily vitamin D supplement and drinking two cups of cow’s milk a day.
1 October 2014
A new study suggests that vitamin D deficiency may be linked to abnormalities of the heart’s electrical activity.