Sensory neurons are activated by stimuli from the environment (such as smells or tastes) and transmit information to the brain and spinal cord. There are also twelve pairs of cranial nerves which emerge directly from the brainstem. These belong to the PNS. They are connected to the muscles and the head’s sensory organs (e.g. eyes, nose and mouth). The PNS is divided into two functional areas: The somatic (or voluntary) nervous system controls all the muscle movements that are under conscious control; the other part, the autonomic (visceral or involuntary) nervous system, controls various activities of the body that are not subject to conscious control via nerves and hormones. These activities include blood pressure regulation, breathing, cell regeneration, heartbeat, digestion, body temperature and metabolism. The control centers of the autonomic nervous system are located in the ganglia (encapsulated collections of nerve cells) found along the spinal column, along the intestine, in the spinal cord, and in the brain. The knowledge necessary for the smooth functioning of the body is stored here. Three nervous systems form the true core of the autonomic nervous system, and they are often equated with it. These are the sympathetic, parasympathetic and enteric nervous systems. The enteric system controls the gastrointestinal system and is sometimes called the “second brain”. Put simply, the sympathetic and parasympathetic divisions are in opposition to each other. While the former prepares the body for action (fight or flight), the parasympathetic division is responsible for relaxing and regenerating the body (rest and digest). Most of the internal organs (e.g. heart, gastrointestinal tract, eyes) are therefore subject to two controls: one acts as the body’s accelerator, the other as the brake. The enteric system is autonomic in the true sense of the word, because in contrast to the sympathetic and parasympathetic systems it is not connected to the CNS. The nerves in the “second brain” have many tasks, such as coordination of intestinal motility, regulation of the immune system and control of fluid and nutrient uptake.
The B vitamins play a key role in the proper functioning of processes in the nerves and brain. Vitamin B1 is required for the provision of energy (glucose) to nerve cells and is involved in the transmission of nervous stimuli (1). The European Food Safety Authority (EFSA) recently confirmed that an adequate supply of vitamin B1 is essential to normal neurological development and function in infants and children up to the age of three years. Vitamin B6 is indispensible for amino acid metabolism and thus for synthesis of the neurotransmitters dopamine, GABA, and in particular serotonin. It is also required for the provision of energy to the nerve cells; sufficient glucose can only be synthesized from proteins and carbohydrates with the aid of vitamin B6. In addition, vitamin B6 is involved in the production of the “myelin sheaths”, the fats that enclose nerve fibers (axons). Vitamin B12 also plays an important part in synthesis of the myelin sheaths. Moreover, it is involved in DNA synthesis and thus in cell division. The concentration of vitamin B12 influences the effectiveness of folic acid (vitamin B9), which is of major significance for the metabolism of myelin components and of neurotransmitters. Like omega-3 fatty acids, folic acid is thought to be of great importance in the development of the nervous system at the start of life.
Minerals, too, influence processes in the nervous system; magnesium and calcium can modulate the transmission of nervous stimuli. The antioxidant trace elements zinc and selenium can probably reduce nerve-damage. Zinc also appears to be involved in the effectiveness of the neurotransmitter GABA (1).
Disease risk reduction
Diseases of the nervous system include stroke, dementia, multiple sclerosis, Parkinson’s disease and epilepsy. According to health reports from the World Health Organization (WHO), these major diseases are responsible for around twelve percent of deaths worldwide and are on the increase, especially in Western industrialized countries. They pose major challenges for health systems (2). But accidents, alcohol abuse and diabetes can also cause neurological damage which can lead to the malfunction or even total loss of function of organs. Prevention is crucial in the fight against the rising incidence of neurological disorders and nerve damage. The following outlines examples of disorders of the nervous system whose risk can be reduced by an adequate intake of micronutrients.
 Vitamins, carotenoids and essential fatty acids, as well as minerals and trace elements play a crucial role, particularly in the development of the nervous system at the start of life and during the aging process. Adequate availability of micronutrients is an essential and indispensible precondition for a well-functioning nervous system, and mental and emotional well-being in humans.
Vitamins, carotenoids and essential fatty acids, as well as minerals and trace elements play a crucial role, particularly in the development of the nervous system at the start of life and during the aging process. Adequate availability of micronutrients is an essential and indispensible precondition for a well-functioning nervous system, and mental and emotional well-being in humans. Nervous system and micronutrient functions
Nervous system and micronutrient functions Multiple sclerosis
Multiple sclerosis Parkinson’s disease
Parkinson’s disease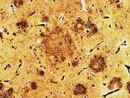 Dementia and depression
Dementia and depression Sensory nerve functions, pain
Sensory nerve functions, pain